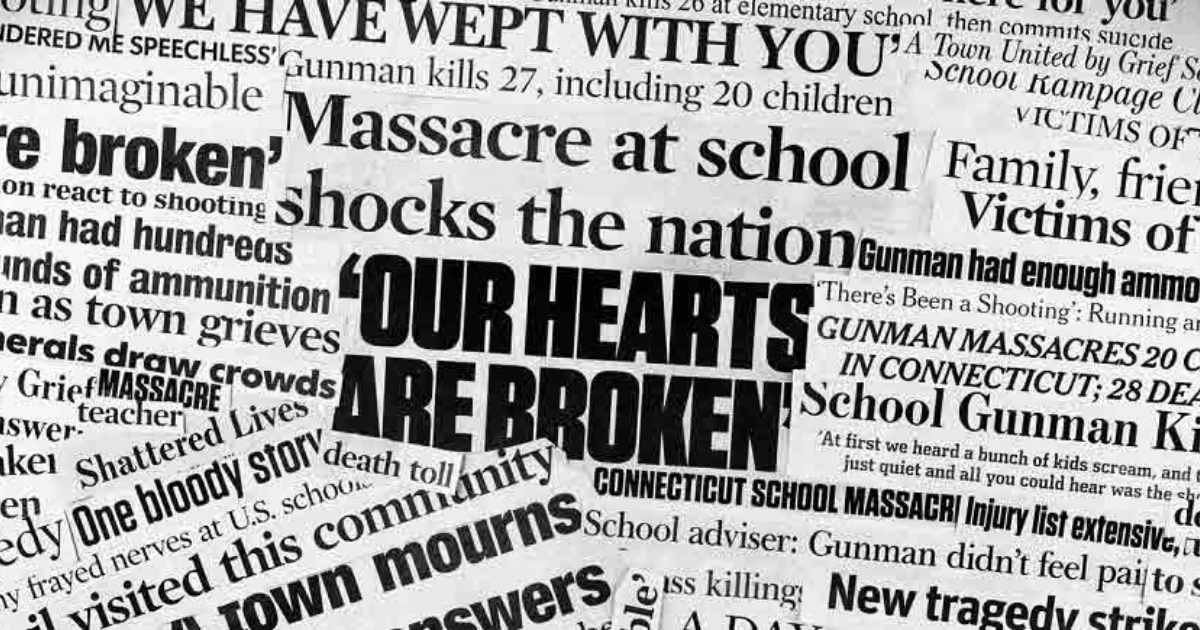
In light of the horrific tragedy that recently transpired in Sutherland Springs, Texas, and the public conversations that ensued, we spoke with Dr. Robin Henderson PsyD, clinical liaison to Well Being Trust, and Chief Executive of Providence Behavioral Health, about the crucial distinction between mental illness and violent criminal behavior. Her message is indispensable.
Let’s be frank, she says. Violent criminal behavior domestic abuse, domestic violence is not a sign or symptom of mental illness. It just isn’t.
Nothing that we know at this point about the suspect’s history is diagnostic of mental illness. Not the shooting. Not domestic violence. Not a discharge from the Air Force for bad conduct. Not the multiple accusations of sexual assault. None of these things are signs or symptoms of mental illness, and it is destructive to claim they are, Dr. Henderson says.
In 2012, while awaiting his court martial, the suspect was held in pretrial confinement at a civilian behavioral health facility, in concern for the risk of harm he may have posed to himself or others; he had previously sneaked guns onto an Air Force base and issued threats against his commanding officers. This, like what little else we know about his life, should not be equated with a confirmation of mental illness. Death threats to his chain of command are more likely equated with his history of violence and assault rather than mental illness, Dr. Henderson says.
When we mislabel violent crime as diagnostic of mental illness, we perpetuate the myth that people suffering with a mental illness, by the whole, are dangerous. And we know that just isn’t true, Dr. Henderson says. In fact, it’s the inverse. Individuals living with mental illness are far more likely to be victims of violence. There’s a preponderance of people with mental health problems who are victims of abuse.
The numbers, as she suggests, are just as clear on the matter. Only 3%-5% of violent crimes can be attributed to individuals who live with a severe mental illness. Compared to the general population, individuals living with severe mental illness are more than 10 times as likely to be victims of violent crime. 1-4 individuals suffering from a mental illness are victims of violence every year.
Inferring that violent criminal behavior is the result of a mental health problem causes so much harm, Henderson says. And the harm is at least twofold.
First, that unfair inference confuses the way we should think about violent criminal behavior in a practical sense. What does this mean? she asks. Do all abusers in domestically violent relationship suffer from mental illness? If violent crime is an indicator of mental health problems, then do we excuse violent criminals by way of mental illness? Of course not.
The second consequence, which is the most concerning to Dr. Henderson and to the rest of us at Well Being Trust, is what this confusion does to inflate stigma and fear. Folks struggling with mental illness don’t have the ability to fight stigma alone, Henderson says. Once we stop perpetuating this myth that mental illness equates to violence, we can really fight stigma, and we can encourage everyone who needs care to seek it out.
Mental health problems, even chronic conditions, are treatable and far more prevalent than commonly perceived. In the U.S. approximately 1 in 5 adults suffer a mental health problem in a given year.
The reality is that individuals with mental health problems are the ones who need protection the most. Dr. Henderson says, We have to separate evil and hate from true illness.